Diabetes Mellitus
"Diabetes is a major life-threatening disease worldwide."

What is Diabetes Mellitus?
Types of Diabetes
2.1.1 Type I Diabetes: It is a chronic disease that develops due to insulin deficiency. It is common in childhood and adolescence, and the most prevalent disease among individuals aged 0 and 18. Generally, it is seen in individuals under 35. The most common age range for onset is 10-15 years. Type I diabetes accounts for approximately 10% of all diabetic patients. In patients with Type I diabetes, uncontrolled hyperglycemia can lead to severe damage to many organs and systems, particularly to the liver and the brain. Symptoms include polydipsia (frequent thirst), polyphagia (frequent hunger), and polyuria (frequent urination). Patients may also have symptoms such as blurred vision, persistent infections, and unexplained weight loss. People with type I diabetes are generally thin and the risk increases if there is a family history of diabetes.
2.1.2 Type II Diabetes: It is also referred to by terms such as “adult-onset diabetes” and “non-insulin dependent diabetes”. It is a disease in which the body cannot respond fully to insulin and also includes insulin resistance. Since there are disruptions in the functioning of the insulin hormone, the level of glucose in the blood gradually increases. Type II diabetes typically occurs later in life. It constitutes approximately 90% of all diabetic patients. These patients are often overweight at diagnosis and often have a strong family history of the disease. Unlike type I diabetes, patients with type II diabetes usually do not show symptoms when diagnosed, and the doctor often makes the diagnosis while investigating another complaint. It is a major social problem affecting millions of individuals across the universe, and its prevalence is increasing faster than expected.
2.1.3 Gestational Diabetes: It is diagnosed in the second or third trimester of pregnancy. It is a disease in which high blood glucose (sugar) levels occur during pregnancy and cause complications for both the mother and the baby. It usually disappears after pregnancy, but affected women or children are at risk of developing type 2 diabetes later in life.
2.1.4 Other types of diabetes: these can result from factors such as infections, diabetes-related syndromes, medications, and chemical agents.
Diabetes Complications
3.1. Acute Complications
3.1.1. Hypoglycemia
3.1.2. Diabetic ketoacidosis
3.2. Chronic Complications
3.2.1. Microvascular Complications
3.2.1.1. Diabetic Retinopathy: Diabetic retinopathy is a complication that causes visual impairment or blindness in most individuals with diabetes as a result of occlusion in the eye vessels and impaired vascular permeability. It is of great importance for these patients to have regular eye checks.
3.2.1.2. Diabetic Nephropathy: It is the loss of function in the kidneys as a result of the deterioration in the structure of the vessels that supply blood to the kidneys. This condition develops due to high blood glucose (sugar). In the United States and our country, approximately half of end-stage renal failure patients are individuals with diabetes. This shows that the most important cause of end-stage renal failure is diabetic nephropathy.
3.2.1.2. Diabetic Neuropathy: Diabetic neuropathy is damage to the nervous system as a result of years of exposure to diabetes. It is a common complication of diabetes that negatively affects the quality of life and creates an economic burden. The main cause of diabetic neuropathy is peripheral vascular disease, damage, and injury to the foot. The most commonly affected areas include the extremities, especially the feet. Nerve damage in these areas is called peripheral neuropathy and can cause conditions such as loss of sensation and widespread pain. It is more important as the loss of sensation can lead to infections and amputations (surgical excision of an organ).
3.2.2. Macrovascular Complications
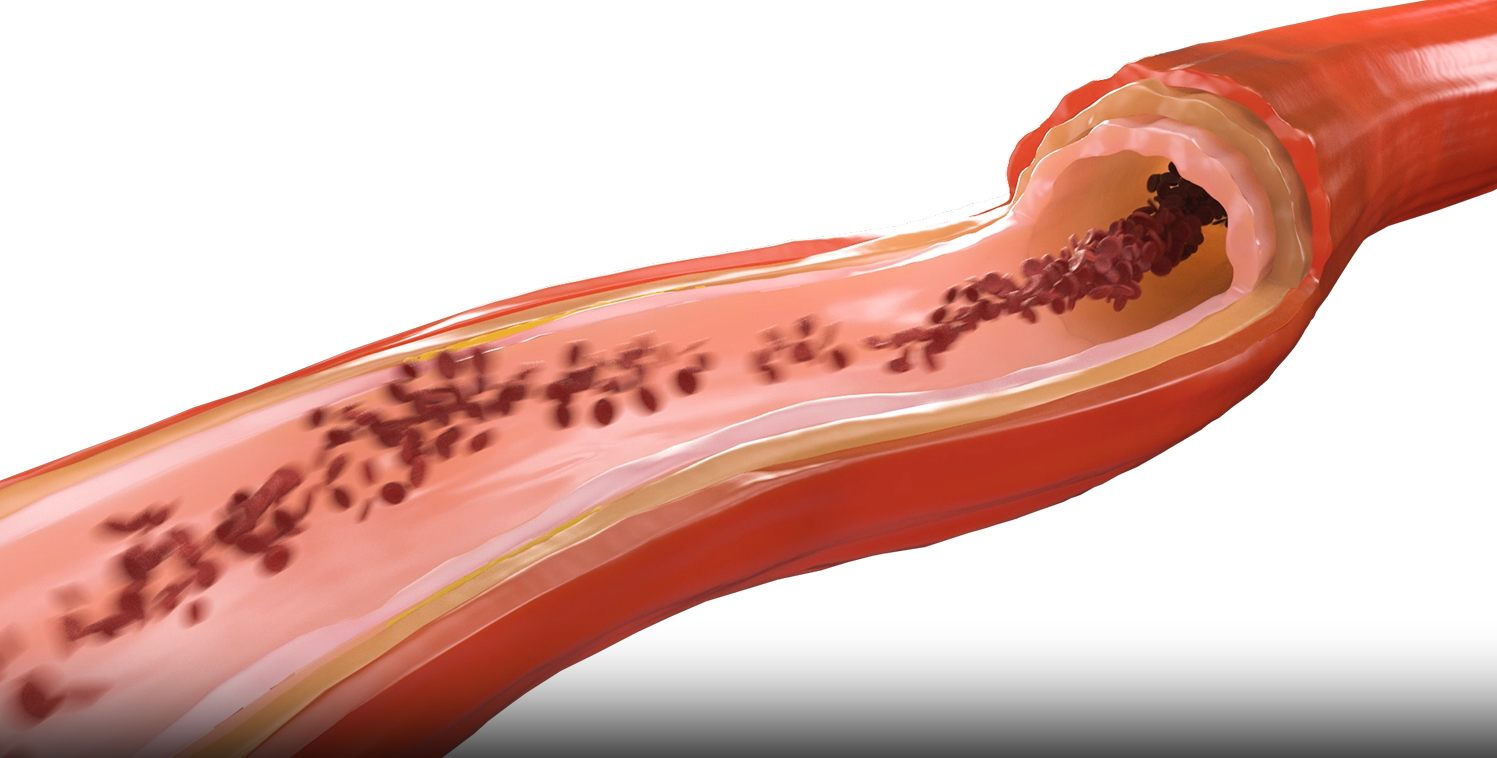
3.2.2.1. Coronary Artery Disease: It is one of the leading diseases in individuals with diabetes. Cardiovascular diseases occur much more frequently in patients with diabetes. The risk of death in diabetic individuals with cardiovascular disease is higher than in other individuals. Cardiovascular diseases seriously reduce the quality of life in patients with diabetes, negatively affect their health, and pose a serious economic, psychological, and social burden to patients. For these reasons, it is very important for individuals with diabetes to control their blood glucose (sugar).
3.2.2.2. Cerebrovascular Disease: The risk of stroke is higher in individuals with diabetes compared to those without diabetes. Decreased insulin secretion in individuals with diabetes causes arteriosclerosis and problems in cerebral (brain) small vessels. Additionally, hyperglycemia may cause vascular damage by reducing cerebral (brain) blood flow.
3.2.2.3. Diabetic Foot: It is a result of neuropathy or peripheral artery disease. It is a leading complication of hospitalizations in individuals with diabetes. If diabetic foot and ulcers (tissue destruction, open wounds) are not treated and cared for properly, they may result in infection, gangrene, amputation, or even death. Diabetic patients; One should be careful against the use of inappropriate shoes and the development of calluses and wounds. In addition, diabetic patients must be educated about foot care and this education must be continued throughout life.
A., Jüni, P., et al., 2023 ESC Guidelines for the management of
acute coronary syndromes. (2023).
Abdissa, S.G., et al., Incidence of heart failure among diabetic
patients with ischemic heart disease: A cohort study. (2020). https://pubmed.ncbi.nlm.nih.gov/32306907/
Ahmed, S., et al., Differences in symptoms and presentation
delay times in myocardial infarction patients with and without diabetes: A
cross-sectional study in Pakistan. (2018). https://pubmed.ncbi.nlm.nih.gov/29716701/
Alaslawi, H., et al., Diabetes self- management apps:
Systematic review of adoption determinants and future research agenda. (2022). https://pubmed.ncbi.nlm.nih.gov/35900826/
Azami, G., et al., Effect of a nurse-led diabetes
self-management education program on glycosylated hemoglobin among adults with
type 2 diabetes. Journal of diabetes research, (2018). https://pubmed.ncbi.nlm.nih.gov/30225268/
Barnes, J. A., et al., Epidemiology
and risk of amputation in patients with diabetes mellitus and peripheral artery
disease. Arteriosclerosis, thrombosis, and vascular biology, (2020). https://pubmed.ncbi.nlm.nih.gov/32580632/
Bhatt, D. L., et al., Diagnosis
and treatment of acute coronary syndromes. (2022). https://pubmed.ncbi.nlm.nih.gov/35166796/
Genuth,
S.M., et al., 3rd Edition. Chapter 1. Classification and diagnosis of
diabetes. Diabetes in America (2018). https://www.ncbi.nlm.nih.gov/books/NBK568014/
https://www.diyabetimben.com/wp-content/uploads/2014/11/turkiyediyabetprogrami.pdf
IDF
Diabetes Atlas, Eighth edition, (2017). https://diabetesatlas.org/atlas/eighth-edition/
Sağlık
Bakanlığı Türkiye Halk Sağlığı Kurumu, Türkiye Diyabet Programı, 2015-2020.
Skyler,
J.S., et al., Differentiation of diabetes by pathophysiology, natural
history, and prognosis. (2017). https://pubmed.ncbi.nlm.nih.gov/27980006/
Squirrell,
D., and Bush, J. Diabetes Mellitus.